Background:
Biallelic TP53 alterations result from either sequence variations or deletions involving TP53 and are not necessarily synonymous with “multi-hit TP53”. According to the 2022 international consensus classification (ICC) for myeloid neoplasms (MN), multi-hit TP53 signifies i) the presence of two or more distinct TP53 mutations, each with variant allele frequency (VAF) ≥10%, ii) a single TP53 mutation with VAF ≥50%, or iii) a single TP53 mutation with VAF ≥10% accompanied by a cytogenetically-apparent del(17p13.1), copy-neutral loss of heterozygosity (LOH) at the 17p TP53 locus, or, in the absence of LOH information, complex karyotype ( Arber et al. Blood 2022;140: 1200). The current study is focused on MN with multi-hit TP53 and examines the additional prognostic impact of morphologic subtype designation, bone marrow (BM) or peripheral blood (PB) blast percentage, TP53 VAF, and MN with diagnostic qualifiers (i.e., therapy-related, or secondary progressing from myelodysplastic/myeloproliferative/overlap syndromes/neoplasms).
Methods:
The current study was conducted under an institutional review board approved minimum risk protocol that allowed retrospective collection and analysis of data from Mayo Clinic patient records. Multi-hit TP53 was defined as per ICC criteria as outlined above ( Arber et al. Blood 2022;140: 1200). Morphologic subtype designations of MN were according to ICC criteria and assigned at the time of TP53 detection. NGS and cytogenetic information was available in all study patients. Survival analyses were calculated from time of TP53 mutation detection. Conventional statistical methods were applied using JMP Pro 16.0.0 software (SAS Institute, Cary, NC, USA).
Results:
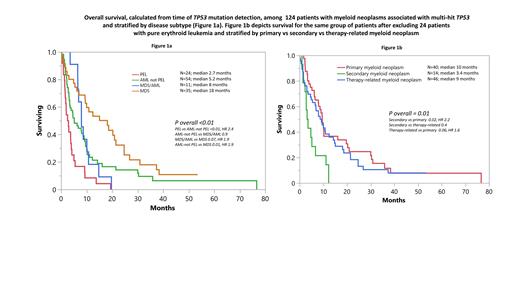
Initial screening flagged 143 patients with biallelic TP53 abnormalities derived from formal laboratory reports of NGS data and cytogenetic studies; of these, 130 met ICC criteria for multi-hit TP53: pure erythroid leukemia (PEL; N=24), acute myeloid leukemia (AML)-not PEL (N=54), myelodysplastic syndromes (MDS; N=36), MDS/AML (N=11), and other MN (N=5). Of these 130 informative cases, 128 (98%) harbored complex/monosomal karyotype (CK/MK). Further analysis excluded patients with “other” MN (N=5) and those without CK/MK (N=2), the latter to mitigate the confounding effect of CK/MK on survival and the former because of small sample size and disease heterogeneity.
Clinical and laboratory characteristics of the 124 study patients are outlined in table 1. Survival analysis stratified by ICC-defined MN subtypes revealed the prognostic relevance of morphological distinction between PEL vs “AML-not PEL” (p<0.01; HR 2.4) and PEL vs “ TP53-muated MDS/AML” (p=0.02; HR 2.3) while survival was similar between “AML-not PEL” and “ TP53-mutated MDS/AML” (p=0.9; Figure 1a). Survival in “ TP53-mutated MDS” was significantly longer, compared to PEL (p<0.01; HR 0.2), “ TP53-mutated AML-not PEL” (p=0.01; HR 0.5), and “ TP53-mutated MDS/AML” (p=0.07; HR 0.5), the latter with borderline significance (Figure 1a). Multivariable analysis confirmed the independent prognostic relevance of ICC subtype designation (p<0.01) and also revealed additional negative prognostic contribution from advanced age (p=0.02), male gender (p=0.02), MN, secondary (p<0.01), MN, therapy-related (p=0.03), and DNMT3A mutation (p=0.02). Significance was retained in all instances, with the exception of MN, therapy-related (p=0.15), when analysis was repeated after excluding PEL cases (Figure 1b).
Conclusions:
The current study confirms the prognostic validity of the ICC morphologic subtype designation and TP53 VAF classification threshold, in the context of multi-hit TP53. The study also highlights the prognostic distinction between PEL and “ TP53-mutated AML-not PEL” and the prognostic alignment between the latter and “ TP53-muated MDS/AML”, both of which displayed inferior survival, compared to “ TP53-mutated MDS”. The study also suggests additional prognostic contribution from secondary and therapy-related qualification while the observation regarding DNMT3A mutation requires validation with higher number of informative cases.
Disclosures
He:Kura Oncology, Inc: Consultancy. Shah:Celgene: Research Funding; MRKR Therapeutics: Research Funding; Astellas: Research Funding; AbbVie: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal